|
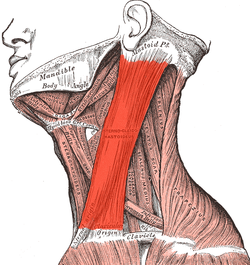
FIG. 1154– The constituent cavernous cylinders of the penis. The glans and anterior part of the corpus cavernosum urethræ are detached from the corpora cavernosa penis and turned to one side. |
|
| The penis is a pendulous organ suspended from the front and sides of the pubic arch and containing the greater part of the urethra. In the flaccid condition it is cylindrical in shape, but when erect assumes the form of a triangular prism with rounded angles, one side of the prism forming the dorsum. It is composed of three cylindrical masses of cavernous tissue bound together by fibrous tissue and covered with skin. Two of the masses are lateral, and are known as the corpora cavernosa penis; the third is median, and is termed thecorpus cavernosum urethræ (Figs. 1154, 1155). |
| The Corpora Cavernosa Penis form the greater part of the substance of the penis. For their anterior three-fourths they lie in intimate apposition with one another, but behind they diverge in the form of two tapering processes, known as the crura, which are firmly connected to the rami of the pubic arch. Traced from behind forward, each crus begins by a blunt-pointed process in front of the tuberosity of the ischium. Just before it meets its fellow it presents a slight enlargement, named by Kobelt the bulb of the corpus cavernosum penis. Beyond this point the crus undergoes a constriction and merges into the corpus cavernosum proper, which retains a uniform diameter to its anterior end. Each corpus cavernosum penis ends abruptly in a rounded extremity some distance from the point of the penis. |
| The corpora cavernosa penis are surrounded by a strong fibrous envelope consisting of superficial and deep fibers. The superficial fibers are longitudinal in direction, and form a single tube which encloses both corpora; the deep fibers are arranged circularly around each corpus, and form by their junction in the median plane the septum of the penis. This is thick and complete behind, but is imperfect in front, where it consists of a series of vertical bands arranged like the teeth of a comb; it is therefore named the septum pectiniforme. |
| The Corpus Cavernosum Urethræ (corpus spongiosum) contains the urethra. Behind, it is expanded to form the urethral bulb, and lies in apposition with the inferior fascia of the urogenital diaphragm, from which it receives a fibrous investment. The urethra enters the bulb nearer to the upper than to the lower surface. On the latter there is a median sulcus, from which a thin fibrous septum projects into the substance of the bulb and divides it imperfectly into two lateral lobes or hemispheres. |
|
 |
FIG. 1155– Transverse section of the penis. |
|
| The portion of the corpus cavernosum urethræ in front of the bulb lies in a groove on the under surface of the conjoined corpora cavernosa penis. It is cylindrical in form and tapers slightly from behind forward. Its anterior end is expanded in the form of an obtuse cone, flattened from above downward. This expansion, termed the glans penis, is moulded on the rounded ends of the corpora cavernosa penis, extending farther on their upper than on their lower surfaces. At the summit of the glans is the slit-like vertical external urethral orifice. The circumference of the base of the glans forms a rounded projecting border, thecorona glandis, overhanging a deep retroglandular sulcus, behind which is the neckof the penis. |
| For descriptive purposes it is convenient to divide the penis into three regions: the root,the body, and the extremity. |
 |
FIG. 1156– Vertical section of bladder, penis, and urethra. |
|
| The root (radix penis) of the penis is triradiate in form, consisting of the diverging crura, one on either side, and the median urethral bulb. Each crus is covered by the Ischiocavernosus, while the bulb is surrounded by the Bulbocavernosus. The root of the penis lies in the perineum between the inferior fascia of the urogenital diaphragm and the fascia of Colles. In addition to being attached to the fasciæ and the pubic rami, it is bound to the front of the symphysis pubis by the fundiform and suspensory ligaments. Thefundiform ligament springs from the front of the sheath of the Rectus abdominis and the linea alba; it splits into two fasciculi which encircle the root of the penis. The upper fibers of the suspensory ligament pass downward from the lower end of the linea alba, and the lower fibers from the symphysis pubis; together they form a strong fibrous band, which extends to the upper surface of the root, where it blends with the fascial sheath of the organ. |
| The body (corpus penis) extends from the root to the ends of the corpora cavernosa penis, and in it these corpora cavernosa are intimately bound to one another. A shallow groove which marks their junction on the upper surface lodges the deep dorsal vein of the penis, while a deeper and wider groove between them on the under surface contains the corpus cavernosum urethræ. The body is ensheathed by fascia, which is continuous above with the fascia of Scarpa, and below with the dartos tunic of the scrotum and the fascia of Colles. |
| The extremity is formed by the glans penis, the expanded anterior end of the corpus cavernosum urethræ. It is separated from the body by the constricted neck, which is overhung by the corona glandis. |
| The integument covering the penis is remarkable for its thinness, its dark color, its looseness of connection with the deeper parts of the organ, and its absence of adipose tissue. At the root of the penis it is continuous with that over the pubes, scrotum, and perineum. At the neck it leaves the surface and becomes folded upon itself to form theprepuce or foreskin. The internal layer of the prepuce is directly continuous, along the line of the neck, with the integument over the glans. Immediately behind the external urethral orifice it forms a small secondary reduplication, attached along the bottom of a depressed median raphé, which extends from the meatus to the neck; this fold is termed thefrenulum of the prepuce. The integument covering the glans is continuous with the urethral mucous membrane at the orifice; it is devoid of haris, but projecting from its free surface are a number of small, highly sensitive papillæ. Scattered glands on the corona, neck, glans and inner layer of the prepuce, the preputial glands, have been described. (*178They secrete a sebaceous material of very peculiar odor, which probably contains casein, and readily undergoes decomposition; when mixed with discarded epithelial cells it is called smegma. |
| The prepuce covers a variable amount of the glans, and is separated from it by a potential sac—the preputial sac—which presents two shallow fossæ, one on either side of the frenulum. |
|
| Structure of the Penis. |
| —From the internal surface of the fibrous envelope of the corpora cavernosa penis, as well as from the sides of the septum, numerous bands or cords are given off, which cross the interior of these corpora cavernosa in all directions, subdividing them into a number of separate compartments, and giving the entire structure a spongy appearance (Fig. 1157). These bands and cords are called trabeculæ, and consist of white fibrous tissue, elastic fibers, and plain muscular fibers. In them are contained numerous arteries and nerves. The component fibers which form the trabeculæ are larger and stronger around the circumference than at the centers of the corpora cavernosa; they are also thicker behind than in front. The interspaces (cavernous spaces), on the contrary, are larger at the center than at the circumference, their long diameters being directed transversely. They are filled with blood, and are lined by a layer of flattened cells similar to the endothelial lining of veins. |
| The fibrous envelope of the corpus cavernosum urethræ is thinner, whiter in color, and more elastic than that of the corpora cavernosa penis. The trabeculæ are more delicate, nearly uniform in size, and the meshes between them smaller than in the corpora cavernosa penis: their long diameters, for the most part, corresponding with that of the penis. The external envelope or outer coat of the corpus cavernosum urethræ is formed partly of unstriped muscular fibers, and a layer of the same tissue immediately surrounds the canal of the urethra. |
 |
FIG. 1157– Section of corpus cavernosum penis in a non-distended condition. (Cadiat.) a.Trabeculæ of connective tissue, with many elastic fibers and bundles of plain muscular tissue, some of which are cut across (c). b. Blood sinuses. |
|
|
| Vessels and Nerves.—The arteries bringing the blood to the cavernous spaces are the deep arteries of the penis and branches from the dorsal arteries of the penis, which perforate the fibrous capsule, along the upper surface, especially near the forepart of the organ. On entering the cavernous structure the arteries divide into branches, which are supported and enclosed by the trabeculæ. Some of these arteries end in a capillary net-work, the branches of which open directly into the cavernous spaces; others assume a tendril-like appearance, and form convoluted and somewhat dilated vessels, which were named by Müller helicine arteries. They open into the spaces, and from them are also given off small capillary branches to supply the trabecular structure. They are bound down in the spaces by fine fibrous processes, and are most abundant in the back part of the corpora cavernosa (Fig. 1157). |
 |
FIG. 1158– Diagram of the arteries of the penis. (Testut.) |
|
| The blood from the cavernous spaces is returned by a series of vessels, some of which emerge in considerable numbers from the base of the glans penis and converge on the dorsum of the organ to form the deep dorsal vein; others pass out on the upper surface of the corpora cavernosa and join the same vein; some emerge from the under surface of the corpora cavernosa penis and receiving branches from the corpus cavernosum urethræ, wind around the sides of the penis to end in the deep dorsal vein; but the greater number pass out at the root of the penis and join the prostatic plexus. |
| The lymphatic vessels of the penis are described on page 713. |
| The nerves are derived from the pudendal nerve and the pelvic plexuses. On the glans and bulb some filaments of the cutaneous nerves have Pacinian bodies connected with them, and, according to Krause, many of them end in peculiar endbulbs (see page 1060). |
 |
FIG. 1159– Veins of the penis. (Testut.) |
|






_.jpg)